Menopause is a natural, transformative phase in a woman’s life, typically occurring between the ages of 45 and 55. While it signals the end of menstruation, menopause involves a host of hormonal shifts that affect various systems in the body.
For many women, this stage often brings symptoms like vaginal dryness, urinary urgency, changes in body composition, and even bone density loss. However, there are proactive ways to navigate these changes and maintain comfort, strength, and vitality. In this post, we’ll explore what to expect during menopause, highlight some lesser-known but impactful challenges, and explain how pelvic floor therapy can be a powerful ally in managing symptoms like pain with intercourse, urinary issues, and the risk of bone loss.
Before we proceed, it is important to note that you will want to consult with your healthcare team before making any changes to your diet or exercise routine so your unique medical history is considered. If you’re in the Denver area and looking for a great team, we’d love to meet with you to discuss your goals!
What Changes Occur During Menopause?
Menopause usually occurs between the ages of 45 and 55, though some women experience it earlier or later. It’s defined by the end of menstruation and is diagnosed after 12 consecutive months without a menstrual period. The hormonal shifts that occur during this time can lead to various physical changes and symptoms, including:
Hot Flashes and Night Sweats
Hot flashes are sudden feelings of warmth, often accompanied by sweating, which can disrupt sleep and lead to daytime fatigue.
Mood Swings and Emotional Changes
Fluctuations in estrogen and progesterone can affect serotonin levels, potentially contributing to mood swings, anxiety, and even depression.
Bone Density Loss
With the decline in estrogen, bones become more vulnerable to thinning, increasing the risk of osteoporosis. Research suggests that resistance training with weights that induce fatigue within 5-8 repetitions can be an effective strategy to maintain bone density.
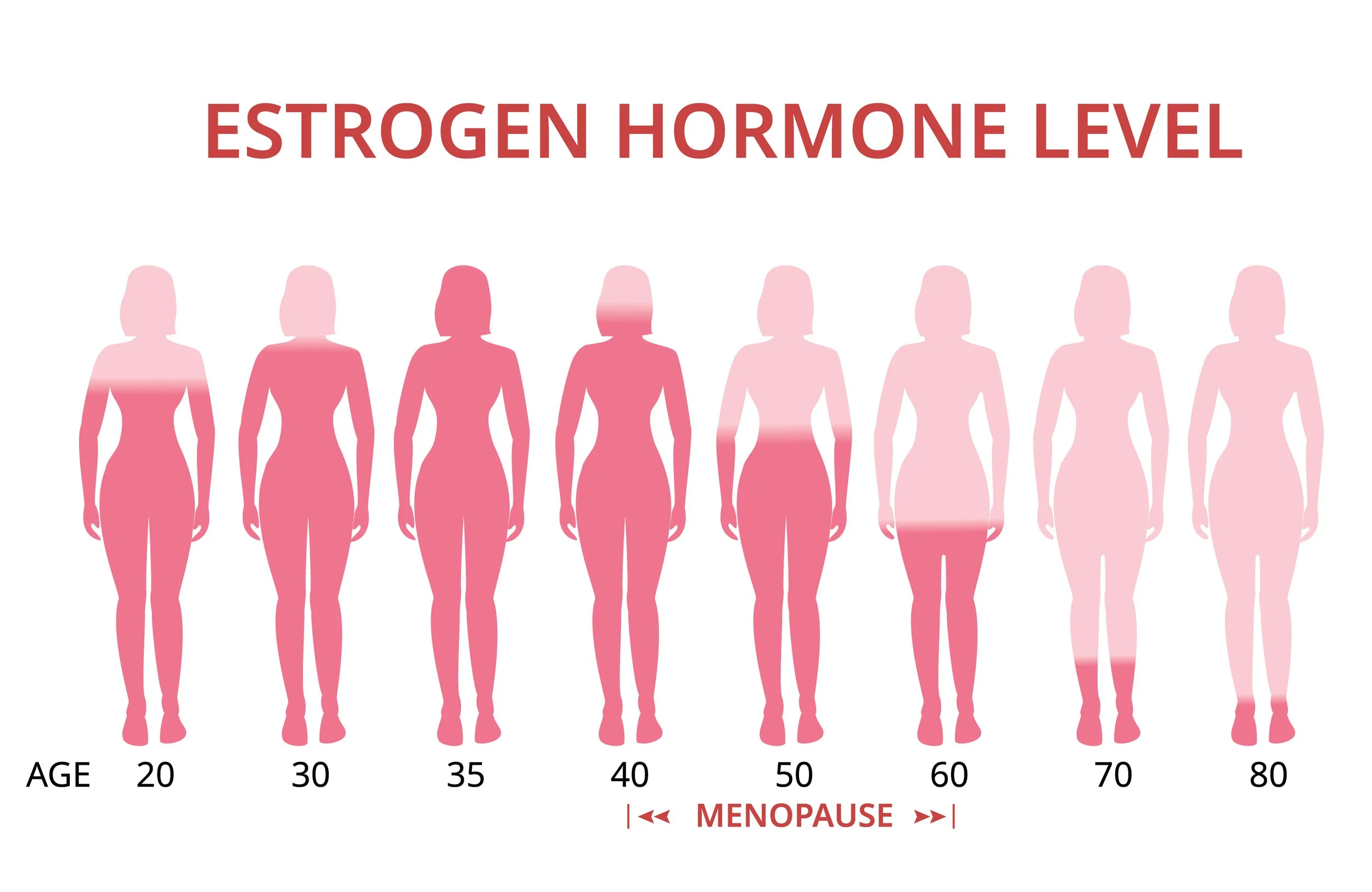
Weight Changes and Slower Metabolism
During menopause, lower estrogen levels can lead to increased fat storage, particularly around the abdominal area. Estrogen also plays a role in regulating insulin, and its decline can raise insulin resistance and A1C levels. Simultaneously, natural muscle mass decline with age slows metabolism. This combination means that even maintaining the same diet and activity level might lead to weight gain. Strength training can combat muscle loss, boost metabolism, and support healthier body composition.
Changes in Sleep Patterns
Night sweats, early awakenings, and other menopausal symptoms often disrupt sleep. Poor sleep quality can increase hunger hormones like ghrelin, heightening cravings and leading to unintentional weight gain.
Increased Stress and Cortisol Levels
Midlife can be a stressful time, and elevated stress levels raise cortisol production. This stress hormone encourages fat storage, particularly in the belly area, compounding the challenges of body composition changes during menopause.
Vaginal Dryness and Discomfort
Decreased estrogen levels can result in less natural lubrication, leading to vaginal dryness and discomfort during intercourse. These changes can also make the vaginal tissues more fragile and susceptible to irritation.
How Pelvic Floor Therapy Can Help Manage Menopausal Symptoms
One of the most overlooked yet powerful tools for managing menopausal symptoms is pelvic floor physical therapy. This specialized area of physical therapy focuses on the muscles, ligaments, and tissues that support the pelvic organs, providing targeted solutions for symptoms often experienced during menopause.
Pain with Intercourse Due to Vaginal Dryness and Pelvic Floor Dysfunction
As estrogen levels drop, tissues in the vaginal and pelvic area may become thinner, drier, and more fragile, leading to discomfort or pain during intercourse. These changes, combined with pelvic floor muscle dysfunction, can make intimacy difficult and even painful.
Pelvic floor physical therapy can address these issues by:
• Improving Blood Flow: Therapeutic exercises and soft tissue techniques can enhance circulation to pelvic tissues, potentially alleviating dryness.
• Releasing Tension: Manual therapy helps relax overactive pelvic muscles that may contribute to pain during intercourse.
• Education and Support: Our therapists provide information on lubricants, techniques, and exercises that support comfort and intimacy. We have products available in office, like Enchanted Rose, a non-hormonal, soothing vaginal balm to help relieve dryness and irritation.
• Identifying Signs of Estrogen Loss: At Klein Physical Therapy, we are trained to identify signs of estrogen loss in the tissues and can help educate patients on whether they might benefit from discussing topical estrogen creams with their doctor. This can be a helpful option to alleviate vaginal dryness and improve tissue health.
Addressing Urinary Urgency and Leakage
Menopause often brings increased urinary urgency and, in some cases, leakage. This is due to both the loss of estrogen, which affects the bladder and urethra, and weakening pelvic floor muscles.
Pelvic floor therapy can be highly effective in managing these symptoms through:
• Strengthening Exercises: Our therapists guide you through specific exercises to build pelvic floor strength, helping you maintain better control.
• Bladder Retraining Techniques: Through gradual and structured approaches, bladder retraining can reduce urgency and improve your ability to hold urine.
• Lifestyle and Dietary Guidance: Minor changes in diet and fluid intake can make a big difference in managing urgency and leakage.
Supporting Bone Health and Combating Muscle Loss
With the decrease in estrogen levels, the risk of osteoporosis rises during and after menopause. Incorporating weight-bearing exercises, particularly those that fatigue the muscles in fewer than 8 reps, is essential for maintaining bone density, reducing fracture risks, and preserving muscle mass.
Our physical therapists can help you:
• Target Key Muscle Groups: Exercises that load the spine, hips, and legs help maintain bone density in areas most vulnerable to osteoporosis.
• Ensure Proper Form and Safety: Our therapists emphasize technique and safe progression, especially if you’re new to weight training.
• Build Sustainable Habits: With regular guidance, we help you develop routines that are both effective and adaptable over time.
Practical Tips for Menopausal Wellness
To thrive during menopause, focus on these key areas:
• Stay Active: Incorporate strength training to build muscle mass, boost metabolism, and support bone health.
• Prioritize Sleep: Develop a calming bedtime routine and keep your bedroom cool (around 65°F) to improve sleep quality.
• Manage Stress: Practice mindfulness, yoga, or breathing exercises to lower cortisol levels, especially upon waking and before bed.
Why Consider Pelvic Floor Physical Therapy?
Our team of experienced pelvic floor physical therapists are dedicated to helping you navigate menopause with confidence and ease. Through personalized assessments and customized therapy plans, we focus on enhancing your comfort, control, and quality of life.
With pelvic floor therapy, our team is able to help you:
• Improve symptoms related to urinary urgency, leakage, and discomfort.
• Enjoy a more comfortable and fulfilling intimate life.
• Strengthen and protect bones, supporting lifelong mobility and wellness.
• Receive guidance on whether topical estrogen creams may be helpful for managing tissue health and vaginal dryness.
Ready to take the next step? Schedule an appointment with one of our pelvic floor specialists today to discuss your unique needs.
While menopause is a natural part of aging, the symptoms associated with it don’t have to disrupt your quality of life. By addressing these changes through targeted strategies like pelvic floor therapy and strength training, you can take charge of your health and wellness during menopause and beyond.
Whether you’re seeking relief from pelvic discomfort, managing symptoms, or working to protect your bones, we’re here to support you every step of the way.
Did you catch our post last month? Check it out here: Understanding Pelvic Floor Dysfunction: Signs, Symptoms, and Solutions