Postpartum Pelvic Floor Rehabilitation
The postpartum period is a transformative time in a person’s life, filled with joy, challenges, and adjustments. Amidst the excitement of welcoming a new baby, it’s easy to overlook the physical toll pregnancy and childbirth take on the body. One crucial aspect of recovery often underestimated is pelvic floor health. Pelvic floor rehabilitation postpartum is not just beneficial—it’s essential for long-term well-being.
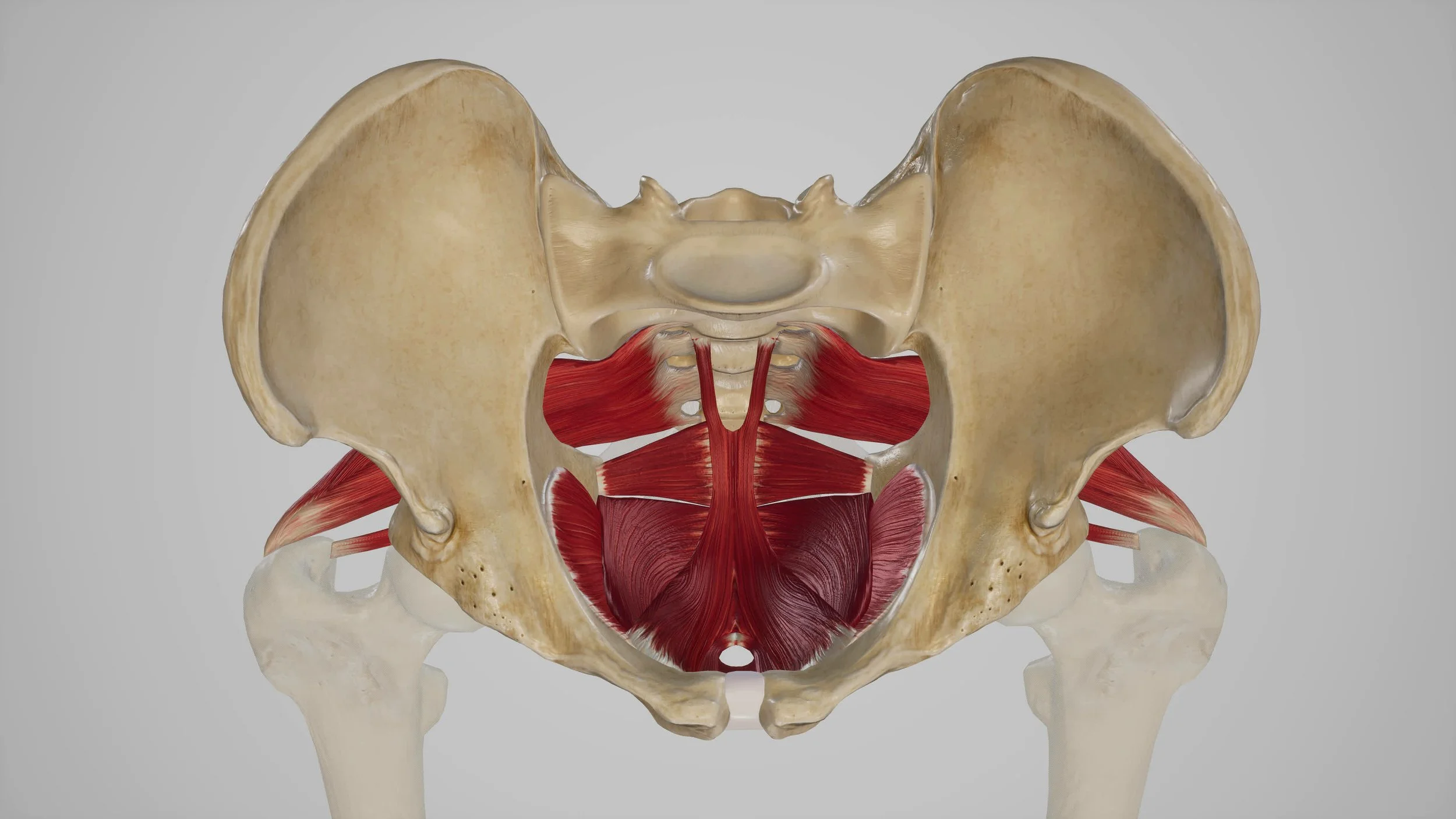
What is the pelvic floor?
The pelvic floor is a group of muscles and connective tissues between the tailbone and pubic bone that support vital organs such as the bladder, uterus, and rectum. These muscles play a critical role in core stability, urinary and bowel control, and sexual function. Pregnancy and childbirth, whether vaginal or cesarean, can weaken or damage the pelvic floor, leading to a variety of issues if left unaddressed.
Common Postpartum Pelvic Floor Issues
Postpartum individuals may experience a range of pelvic floor-related concerns, including:
1. Urinary Incontinence
Leaking urine during activities like coughing, sneezing, or exercising is a common postpartum issue (stress incontinence). Another form is urge incontinence when urine is leaked during a strong urge.
2. Pelvic Organ Prolapse
This occurs when pelvic organs shift downward due to inadequate support, often resulting in pressure or discomfort.
3. Pain and Discomfort
Pain during intercourse, lower back or SIJ pain, or a sensation of heaviness in the pelvic area can stem from pelvic floor dysfunction.
4. Diastasis Recti
A separation of the abdominal muscles, which often coincides with weakened pelvic floor muscles and affects core stability.
The Importance of Rehabilitation
Pelvic floor rehabilitation focuses on restoring strength, flexibility, and function to the pelvic muscles. Here’s why it’s crucial:
1. Improved Bladder and Bowel Control
Strengthening and improving the coordination of the pelvic floor can alleviate or prevent incontinence and improve overall quality of life.
2. Prevention of Long-Term Issues
Addressing pelvic floor dysfunction early can reduce the risk of chronic pain, pelvic organ prolapse, urinary incontinence and other complications later in life.
3. Enhanced Core Stability
A strong pelvic floor contributes to overall core strength, which supports posture and reduces the risk of injury.
4. Better Sexual Health
Rehabilitation can address pain or discomfort during intimacy and improve sexual satisfaction.
Tips for Initial Healing of Perineal Tearing
Over 85% of women who deliver vaginally will have some degree of perineal tearing, and proper care is essential for healing. Here are some tips to promote recovery:
1. Practice Good Hygiene
Keep the area clean by using warm water to rinse the perineal area after using the bathroom. Use a peri bottle for gentle cleansing.
2. Apply Cold Compresses
Ice packs or chilled pads (padsicles) can reduce swelling and provide pain relief in the initial days postpartum.
3. Use Pain Relief Options
Over-the-counter pain relievers, as recommended by your healthcare provider, can help manage discomfort. Topical anesthetics may also be beneficial.
4. Rest and Avoid Strain
Minimize activities that put pressure on the perineal area, such as heavy lifting or prolonged sitting.
5. Consider Sitz Baths
Soaking in a warm, shallow bath can soothe the area and promote healing. Add Epsom salt for added relief if approved by your provider.
6. Stay Hydrated and Eat Fiber-Rich Foods
Prevent constipation by drinking plenty of water and consuming a high-fiber diet. Straining during bowel movements can worsen discomfort.
7. Consult Your Healthcare Provider
Follow up with your healthcare provider to monitor healing and address any concerns, such as signs of infection or severe pain.
What Does Pelvic Floor Rehabilitation Involve?
Rehabilitation typically begins with an assessment by a specialized physical therapist who can tailor a program to your specific needs. Common elements include:
Pelvic Floor Exercises: Are kegels right for you? Learning how to coordinate the pelvic floor with breathing and functional activities is key and often involves learning how to lengthen and relax your pelvic floor first.Your PT will help determine if pelvic floor contractions, also known as Kegels, will be a part of your plan of care.
Breathing Techniques: Proper breathing can help coordinate the diaphragm and pelvic floor, enhancing muscle function.
Whole body strengthening and improving posture: Your PT will guide you on returning to exercise which may include a return to running program. Generally your medical provider will clear you for all activity at 6 weeks postpartum which you may not be ready for. PT will include integrating core and pelvic floor with your entire system in order to prepare your body for higher impact activities like running or HIIT exercise. Running is not typically recommended until 12 weeks postpartum.
Manual Therapy: Hands-on techniques may be employed to release tension or address scar tissue from tears, cesarean section scars or episiotomies. Dry needling may also be used.
When to Start Rehabilitation
If you are having pain or would like to have guidance on exercise in the first few weeks after having a baby, you can start any time postpartum- even before 6 weeks! An internal pelvic exam would be held until 6 weeks so that a medical provider can provide clearance that tissues have healed. It is never too late to seek help. Even years after giving birth, addressing pelvic floor health can yield significant benefits.
Conclusion
Pelvic floor rehabilitation is an investment in your health, enabling you to recover fully and enjoy your postpartum journey without unnecessary discomfort or limitations. Prioritize this aspect of self-care—your body will thank you for it. All of our therapists at Klein Physical Therapy specialize in postpartum rehabilitation. We offer hour-long sessions to have time to address your entire body and provide one-on-one care. Book your appointment today!