Hip pain can slow you down - whether you’re an athlete, a weekend warrior, or just trying to sit comfortably at your desk. One often-overlooked cause of chronic hip pain is Femoroacetabular Impingement (FAI), or hip impingement. It affects both men and women, and unfortunately, it’s often misunderstood or dismissed until symptoms become more severe.
If you’re experiencing groin discomfort, hip stiffness, or pain with sitting or movement, you may be dealing with FAI and physical therapy can play a key role in helping you recover.
What Is Femoroacetabular Impingement (FAI)?
Femoroacetabular impingement (FAI) occurs when there’s abnormal contact between the ball (femoral head) and socket (acetabulum) of the hip joint. This causes friction that can damage cartilage and limit joint movement over time. FAI can lead to pain during activity or even while sitting still, and is a major contributor to chronic hip discomfort.
Types of FAI:
CAM impingement – Excess bone on the femoral head
Pincer impingement – Extra bone on the acetabulum (socket)
Combined impingement – A mix of both types
These structural changes can lead to stiffness, catching, or sharp pain in the hip, especially during deep movements like squatting or lunging.
Symptoms of Hip Impingement
Hip impingement can cause a variety of symptoms, including:
Sharp or aching hip or groin pain
Pain with sitting, squatting, or twisting
Decreased hip mobility
Clicking or catching sensation in the hip
Pain that radiates into the lower back or pelvic region
In many cases, people with FAI also experience pelvic floor dysfunction, which often goes unrecognized.
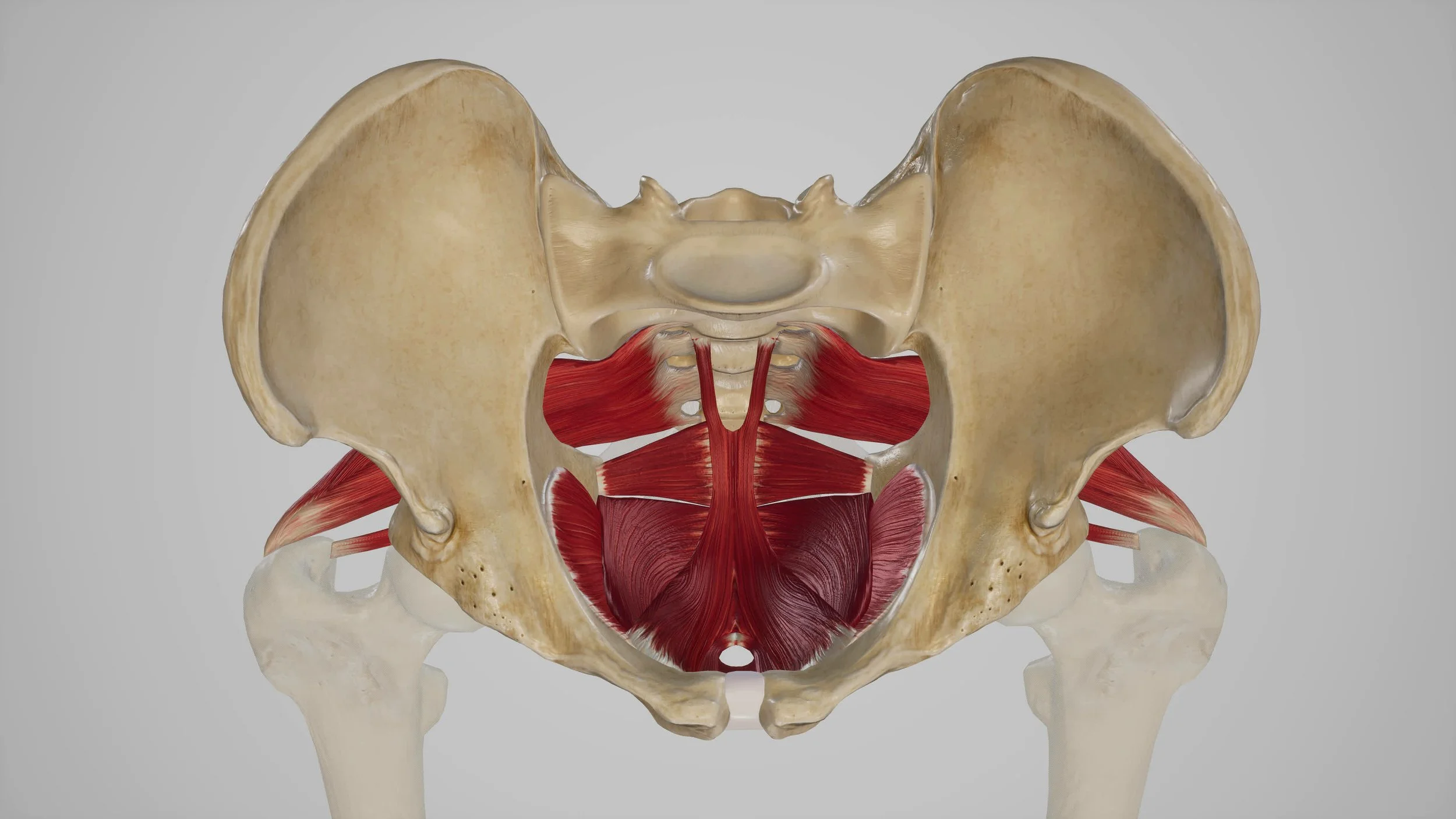
How Hip Impingement Affects the Pelvic Floor
Because the hips and pelvis work as a unit, chronic hip dysfunction can lead to compensations in the pelvic floor muscles. This is true for both men and women.
You may notice:
Groin or pelvic pain
Urinary urgency
Tailbone pain or tension
Discomfort with prolonged sitting
Pain with intimacy or sexual activity
At Klein Physical Therapy, our team is uniquely trained to identify and treat these overlapping symptoms through pelvic floor physical therapy, giving you a more complete and lasting recovery.
Physical Therapy for Hip Impingement (FAI)
There isn’t a one-size-fits-all approach to FAI, which is why personalized care is key. At Klein Physical Therapy, we take the time to assess how your hip, pelvis, and whole body are working together, and build a treatment plan just for you.
Your FAI Physical Therapy Treatment May Include:
Manual therapy including hip mobilizations to improve joint mobility and relieve tightness
Dry needling and myofascial release to reduce muscle tension and restore movement
Pelvic floor physical therapy to address related pelvic dysfunction
Hip and core strengthening exercises for better stability and alignment
Movement retraining to restore natural function and prevent further irritation
We focus on treating the root cause of your pain—not just the symptoms—so you can get back to doing the things you love.
Why Choose Klein Physical Therapy?
At Klein Physical Therapy, we provide compassionate care for a variety of conditions, specializing in pelvic health (for both men and women), women’s health, spine physical therapy, and whole-body wellness. Our evidence-based, hands-on approach allows us to address hip impingement through the lens of pelvic floor physical therapy - a highly effective approach.
Our team works with all genders, and we are passionate about creating a welcoming space where you feel heard, supported, and empowered.
Ready to Get Started with Hip Impingement Physical Therapy in Denver?
If you suspect you’re dealing with hip impingement or femoroacetabular impingement (FAI), don’t wait for the pain to get worse. Our team at Klein Physical Therapy is here to help you move with confidence again.
Located in Denver, Colorado’s South Downing Business and Wellness District